Plastic surgery is the art of reshaping and repairing various parts of the body. This surgical discipline focuses both on solving functional (physiological) problems and improving aesthetic (visual) appearance. Its fundamental goal is to restore bodily integrity and enhance a person’s quality of life—whether the issue is tissue loss caused by an accident, a congenital difference, or changes that occur over time. Advanced surgical techniques are used to bring body structures to the most ideal form and function.

EFC CLINIC is a center of excellence specializing in the most meticulous fields of surgical medicine, from aesthetic surgery to interventional treatments—where every step progresses with refined attention. Medical excellence, aesthetic precision, and uncompromising ethical standards converge on the same path. Our subspecialty-trained experts aim to achieve natural and reliable results by delivering evidence-based care supported by modern imaging, standardized protocols, and safety systems. From consultation to recovery, your care is coordinated end-to-end with clear communication, transparent planning, and genuine respect for your health.
Are the Fields of Plastic Surgery Limited to Aesthetics Only?
Although aesthetic or cosmetic surgery is the first thing that comes to mind when plastic surgery is mentioned in society, this is actually a much broader umbrella. Plastic surgery basically encompasses two main subspecialty areas: Reconstructive surgery and Cosmetic (aesthetic) surgery.
What Is Reconstructive Surgery?
Reconstructive surgery, by definition, focuses on “abnormal” or functionally impaired structures of the body. The primary clinical aim here is to restore normal function and appearance by correcting congenital defects, injuries caused by accidents, infections, or diseases (such as cancer).
Some common examples of reconstructive surgery are as follows:
- Cleft lip and palate repair
- Breast reconstruction after breast cancer
- Correction of contractures (tightening) after severe burns
- Replantation of amputated limbs after trauma
- Reconstruction of tissue loss after tumor removal
From a clinical and administrative perspective, reconstructive surgery is generally considered “medically necessary” and is therefore evaluated within the scope of health insurance.
What Is Cosmetic (Aesthetic) Surgery?
In contrast to reconstructive surgery, cosmetic surgery is performed to reshape or alter “normal” structures of the body. The purpose of cosmetic surgery is entirely aesthetic; the sole goal is to improve the patient’s current appearance and change their form.
Some common cosmetic procedures include:
- Breast augmentation or reduction
- Liposuction (Fat removal)
- Abdominoplasty (Tummy tuck)
- Rhytidectomy (Facelift)
- Rhinoplasty (Nose surgery)
Since cosmetic surgery is not considered medically necessary, it is classified as an “elective” procedure and is generally not covered by health insurance.
Is the Boundary Between Aesthetics and Reconstruction in Plastic Surgery Always Clear?
Bringing these two areas together is the core identity of plastic surgery. However, in practice, the distinction between “reconstructive” and “cosmetic” is often unclear. This ambiguity can create challenges in both clinical classification and insurance reimbursements.
Rhinoplasty (nose surgery) is the most classic example of this ambiguity.
A rhinoplasty performed solely to “improve the appearance of the nose” is classified as “cosmetic.” However, the exact same surgical procedure required to “restore normal breathing and normal appearance after a severe nasal fracture” is classified as “reconstructive.”
This shows that classification depends not on the surgical technique itself but on the cause of the defect (e.g., congenital/traumatic vs. normal anatomy) and the primary aim (restoring function vs. improving appearance).
Who Is the Right Candidate for Cosmetic Surgery?
Cosmetic surgery is performed to improve a patient’s “appearance and self-confidence.” For patients seeking aesthetic procedures, the primary motivation is usually dissatisfaction with body image. Therefore, patient selection requires not only a physical assessment but also an evaluation of the patient’s psychological state and motivations.
What Is the Role of Psychological Assessment?
A critical component of the consultation before an aesthetic procedure is a comprehensive psychological assessment. The primary purpose of this assessment is to identify “patient types” or forms of psychopathology that may pose a barrier to surgical intervention.
One of the primary concerns is Body Dysmorphic Disorder (BDD). Patients with BDD may have unrealistic expectations that cannot be corrected surgically or a distorted perception of their “normal” anatomy. In such cases, these patients may be better treated by a mental health professional rather than a cosmetic surgeon. This psychological assessment is an ethical and clinical responsibility based on the surgeon’s individual judgment.
What Are the Common Complications of Plastic Surgery?
Like all surgical specialties, plastic surgery inherently carries risks.
Like all operations, plastic surgery also carries certain risks. The most common potential complications include:
- Surgical site infection
- Hematoma (Blood collection)
- Seroma (Fluid collection)
- Wound edge separation
- Tissue death (necrosis)
- Venous thromboembolism (VTE)
Hematoma and seroma are common wound collections that can jeopardize surgical outcomes.
Why Is the Risk of Venous Thromboembolism (VTE) So Important?
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is one of the most serious and life-threatening potential complications in plastic surgery. The risk is not the same for all procedures; abdominoplasty (tummy tuck), in particular, is described as “one of the highest-risk plastic surgery procedures for venous thromboembolism.”
Therefore, it is critically important to determine the patient’s clot risk using tools such as the Caprini scoring system. In high-risk patients, preventive measures (prophylaxis) with blood-thinning (anticoagulant) medications may be required.
However, this creates a critical clinical conflict, especially in high-risk cosmetic procedures. Procedures with the highest clot risk, such as tummy tucks, also involve “large raw surface areas and tissue separation (dissection).” This extensive dissection can significantly increase the risk of hematoma or bleeding, making “preoperative use of blood thinners” risky.
At this point, the surgeon must make a difficult clinical decision: reducing clot risk with blood thinners can cause a direct surgical complication (hematoma), which may jeopardize tissue health or require repeat surgery.
Contact us now to get detailed information about our treatments and procedures and to schedule an appointment!
How Is a Facelift (Rhytidectomy) Performed?
The facelift procedure has undergone significant evolution over the years. Early techniques in the early 1900s were based solely on excising excess skin. However, methods based only on tightening the skin would lose their effect over time due to the “natural elasticity of the skin.” This limitation pushed surgeons to explore deeper layers beneath the skin to achieve a more durable and natural-looking rejuvenation.
What Is the SMAS Technique?
The fundamental milestone in modern facelift surgery was the anatomical definition of the SMAS (Superficial Musculoaponeurotic System) in 1976. The SMAS is a distinct fascial (connective tissue) layer located just beneath the skin, continuous with the muscles of the neck, and enveloping the facial expression muscles.
In SMAS techniques, after the skin is elevated, this underlying SMAS layer is manipulated. There are two main methods: folding the SMAS onto itself (plication) or excising a portion of it and tightening it (SMASectomy). These techniques are primarily used to correct jowling along the jawline and neck laxity caused by sagging cheeks.
What Is a Deep Plane Facelift?
The further evolution of facelift surgery involved moving the surgical plane deeper, into the sub-SMAS plane. This is the critical difference in these techniques. It allows the surgeon to elevate the SMAS, the overlying cheek fat, and the skin as a single integrated unit. A deep plane facelift permits complete elevation and re-suspension of the midface by releasing the key retaining ligaments of the face.
Which Facelift Technique Is Better?
This remains a debated topic among surgeons. Deep plane techniques offer the advantage of tension-free skin closure because the lift is anchored to deeper tissues, and they may be more effective at elevating the midface.
However, these benefits come with increased technical difficulty. Sub-SMAS dissection is more complex, carries “greater risk to the facial nerve,” and generally requires a longer recovery period. While some studies support superior outcomes with the deep plane, other studies have found no significant long-term difference. This suggests that meticulous execution of the chosen technique and the surgeon’s experience may be more critical than the specific plane of dissection.
How Is Eyelid Surgery (Blepharoplasty) Performed?
Upper eyelid surgery generally involves removing excess skin (dermatochalasis), lax muscle, and herniated fat pads:
The lower eyelid is more complex, and the approach is determined by the patient’s primary complaint.
Which Methods Are Used in Lower Eyelid Surgery?
There are two main approaches in lower eyelid surgery, and the choice depends on the patient’s anatomy:
Transcutaneous (External Incision) Approach: The incision is made through the skin just below the lash line (approximately 1 mm). This approach is primarily used for patients with excess lower eyelid skin and skin/muscle laxity. It allows direct removal of excess skin, but due to the vertical scar and tension, it carries a higher risk of postoperative lower lid malposition (e.g., ectropion—outward turning of the lid).
Transconjunctival (Internal Incision) Approach: This is an internal approach. The incision is made through the conjunctiva on the inside of the lower eyelid, so there is no external scar. This approach is primarily indicated for patients (usually younger) who do not have significant excess skin but complain of herniated orbital fat pads (“bags”). It leaves no visible scar and carries minimal risk of lid retraction.
What Is the Modern Concept in Eyelid Surgery?
The philosophy of modern eyelid surgery has undergone a significant change. “Historically, lower eyelid surgery was a reductive procedure focused on removing skin, muscle, and fat.” This aggressive approach often resulted in a “hollow” and “operated-on” appearance around the eyes.
The “new concept” or “modern eyelid surgery,” instead, focuses on “preserving periorbital volume.” This is achieved through “fat preservation and repositioning.” In this technique, herniated orbital fat is not removed; instead, it is advanced and spread over the orbital rim to fill the tear trough. This represents a fundamental shift in understanding, treating periorbital aging not merely as tissue excess but as volume loss and descent.
What Are the Open and Closed Approaches in Rhinoplasty (Nose Surgery)?
This is one of the most frequently asked questions by patients and represents a surgical trade-off: Exposure (Visibility) vs. Tissue Preservation.
Open (External) Rhinoplasty Approach
In this technique, in addition to intranasal incisions, a small incision is made across the skin bridge between the two nostrils (the columella). This allows the surgeon to fully elevate the nasal skin and directly visualize the underlying cartilage and bony framework.
The open approach is preferred when the surgeon needs to see the nasal framework. Main reasons include:
- Complex nasal tip deformities
- Extensive dorsal modification
- Severe nasal deviations
- Structural repairs requiring grafts (cartilage grafting)
Closed (Endonasal) Rhinoplasty Approach
In this approach, all incisions are made inside the nostrils. There is no visible external scar. The surgeon reaches the nasal framework by working through these internal incisions.
The closed approach is used for less extensive changes and in cases where preservation of the soft tissue envelope is important:
- Simpler nasal tip issues
- Minimal dorsal intervention
- Thin-skinned patients
The open approach sacrifices a scarless result (by leaving a small scar on the columella) in exchange for maximum visibility of the surgical framework. The closed approach preserves the columella but limits visibility. The surgeon’s decision is strategic: Is the deformity complex enough to require the full exposure provided by the open approach?
What Is Preservation Rhinoplasty?
Preservation rhinoplasty is a surgical philosophy that can be applied to both open and closed approaches and emphasizes “osteocartilaginous preservation.” Instead of aggressively “breaking and removing” the dorsal hump, “impaction” techniques (lowering by removing underlying support tissues) are often used to reduce the nasal dorsum while preserving its natural structural integrity.
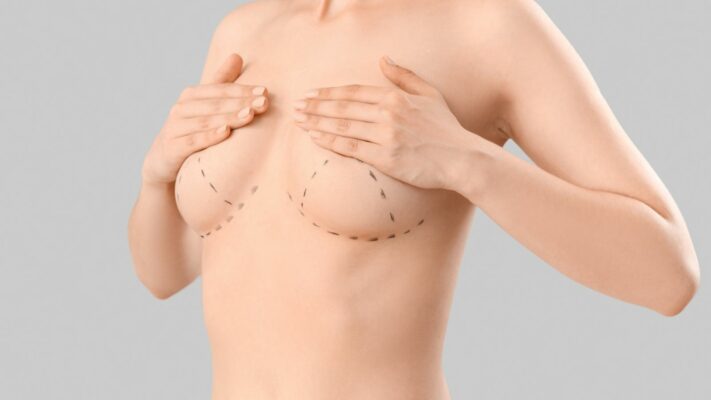
What Is Considered in Breast Augmentation Surgery?
When planning breast augmentation surgery, two key decisions are made: the type of implant (silicone or saline, smooth or textured surface) and where the implant will be placed.
What Is the Implant Placement Plan?
There are two main anatomical pockets where the implant can be placed:
- Subglandular (Above the muscle): The implant is placed behind the breast gland but in front of the chest muscle (pectoralis major).
- Submuscular (Below the muscle): The implant is placed partially or completely behind the chest muscle.
What Is the Most Common Complication of Breast Augmentation Surgery?
Capsular contracture (CC) is described as “the most common complication” after implant-based breast surgery. It is defined as an “excessive fibrotic (hardening) foreign body reaction” to the implant. This process leads to the formation of a thick, fibrous capsule (membrane) surrounding the implant. Over time, this capsule tightens, causing the breast to feel firm, painful, and aesthetically distorted.
For symptomatic (severe) CC, the “gold standard” treatment is surgical intervention (capsulectomy—removal of the capsule). However, even surgical management has a “significant recurrence rate.”
Contact us now to get detailed information about our treatments and procedures and to schedule an appointment!
How Can the Risk of Capsular Contracture Be Reduced?
Evidence shows that certain factors are known to increase risk. When these factors come together, the risk profile rises:
- Subglandular (above the muscle) placement
- Smooth-surfaced implants
- Silicone-filled implants (compared to saline)
This creates a clear decision tree for the surgeon. It can be said that the highest-risk configuration is a smooth-surfaced silicone implant placed in the above-the-muscle plane. Conversely, the evidence-based configuration to minimize CC risk is a textured-surface implant placed in the below-the-muscle plane.
How Are Breast Lift (Mastopexy) and Reduction Surgery Planned?
When planning a mastopexy (lift) or reduction surgery, the surgeon must solve two separate anatomical problems at the same time: (1) reshaping the skin envelope (the skin “bra”) to correct ptosis and reduce volume, and (2) repositioning the nipple–areola complex (NAC) on a living vascular pedicle (pedicle) to preserve viability.
Which Incision Patterns Are Used for the Skin Envelope?
The incision pattern used is selected according to the degree of ptosis and the amount of reduction:
- Periareolar (Around the areola only)
- Vertical (“Lollipop” incision)
- Wise Pattern (“Inverted-T” or “anchor” incision)
The periareolar incision leaves the least scarring but is only for mild ptosis. The vertical incision provides good projection for moderate ptosis. The Wise pattern leaves the most scarring but provides maximum control in the most severe ptosis and large-volume reductions.
How Is Nipple Viability (Pedicle) Preserved?
The “pedicle” is the vital “vascular stalk” consisting of glandular tissue, fat, and blood vessels that is preserved and mobilized to maintain the viability and sensation of the Nipple–Areola Complex (NAC).
Different pedicle techniques are used to preserve the blood vessels supplying the nipple. The main ones are:
- Inferior (Lower) Pedicle
- Superomedial (Upper-inner) Pedicle
- Superior (Upper) Pedicle
For example, a common and reliable procedure is the combination of “Superomedial pedicle with Wise-pattern (Inverted-T) skin resection.”
How Is Breast Reconstruction Performed After Mastectomy?
There are two main routes for breast reconstruction after mastectomy (removal of the breast): implant-based reconstruction or autologous (the patient’s own tissue) reconstruction.
What Are the Advantages and Disadvantages of Implant-Based Reconstruction?
This is the most common approach. Its popularity stems from technical simplicity and, most importantly, the “absence of donor-site morbidity.”
However, implants carry long-term risks such as capsular contracture and implant rupture. More importantly, implant-based reconstruction has “higher complication rates in irradiated (radiation-treated) fields,” which makes it a less preferred option for patients expected to receive radiotherapy after mastectomy.
What Is Reconstruction Using the Patient’s Own Tissue (Autologous Flap)?
Autologous reconstruction uses the patient’s own tissue (usually from the abdomen, back, or thigh) to create a “natural,” soft, and durable breast mound. It is the preferred method in patients expected to undergo radiation therapy.
What Is the Difference Between a TRAM Flap and a DIEP Flap?
This is the best example showing the evolution of autologous reconstruction. Both typically use the skin and fat of the lower abdomen to create a new breast, but there is a vital difference between them:
- Pedicled TRAM Flap: This is an older technique. A large ellipse of skin and fat from the lower abdomen is harvested together with part or all of the underlying rectus abdominis muscle. This entire unit is tunneled under the skin to reach the chest while remaining attached to its blood supply.
Disadvantage: The primary disadvantage is significant donor-site (abdominal) morbidity. Sacrificing the rectus muscle results in high rates of abdominal wall weakness, bulging, and hernia (up to 16%).
- DIEP Free Flap: This is the preferred method in modern practice and is a “muscle-sparing” technique.
Method: Like TRAM, this flap uses the skin and fat of the lower abdomen. However, the surgeon meticulously dissects the small blood vessels (perforators) that supply that skin and fat through the muscle using microsurgery, leaving the muscle completely in place. The flap is then transferred to the chest (separated from its blood supply), and the flap vessels are reconnected (anastomosed) to recipient vessels in the chest under the microscope.
Advantages: This technique provides the same “natural” tissue as the TRAM flap but minimizes abdominal donor-site morbidity (about 1% hernia rate) by preserving the entire abdominal muscle.
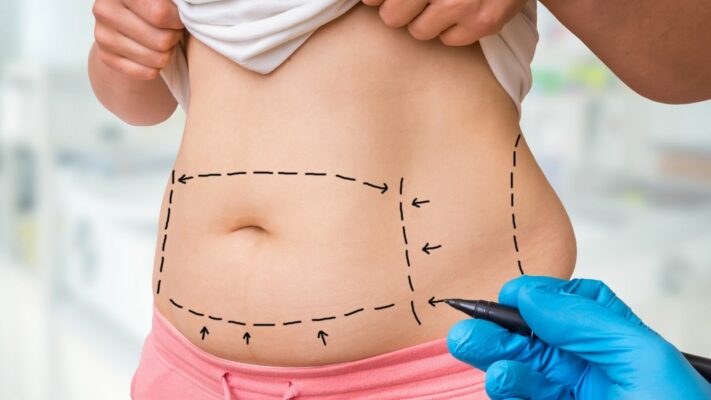
Who Is Abdominoplasty (Tummy Tuck) Surgery Suitable For?
Abdominoplasty is a surgical procedure designed to correct two main anatomical problems: excessive skin laxity and separation of the rectus abdominis muscles (diastasis recti). These conditions typically occur after pregnancy or massive weight loss.
What Is the Difference Between a Full and a Mini Tummy Tuck?
The extent of the surgery is determined by the severity of the problem, and there are two main types:
- Full Abdominoplasty
- Mini Abdominoplasty
A full tummy tuck is required for significant laxity and muscle separation (diastasis recti) in both the lower and upper abdomen. In this procedure, the muscles are usually repaired (plication) and the belly button is moved to a new position. A mini tummy tuck is suitable for patients with mild laxity only in the lower abdomen and generally without muscle separation. This is a more limited procedure, and the belly button is not altered.
What Is Lipoabdominoplasty?
Lipoabdominoplasty represents a modern evolution that combines liposuction with abdominoplasty skin excision. In this technique, traditional wide undermining of the abdominal flap is avoided. Instead, liposuction is used for “lipo-dissection.” This approach preserves Scarpa’s fascia and, most importantly, the abdominal wall perforator vessels that supply blood to the flap. By preserving this robust blood supply and minimizing the “dead space” created by wide undermining, lipoabdominoplasty has been shown to have a lower complication rate, especially for seroma (fluid collection).
What Are the Differences Between Liposuction Methods?
Liposuction can be performed using different technologies. The main methods are as follows:
- Suction-Assisted Lipoplasty (SAL) – Conventional Method
- Ultrasound-Assisted Lipoplasty (UAL / VASER) – Ultrasound Energy
- Power-Assisted Lipoplasty (PAL) – Mechanical Vibration
SAL is the physical breakdown and aspiration of fat using manual back-and-forth movements of the cannula following tumescent fluid infiltration. PAL uses a handpiece that rapidly vibrates the cannula mechanically; this reduces surgeon fatigue and speeds the procedure, especially in large-volume or firm (fibrous) areas.
VASER (UAL) is a “fat pre-treatment” device. It uses a special probe that emits high-frequency ultrasonic energy to selectively emulsify (liquefy) fat before aspiration.
Why Is “High-Definition” Liposculpture (Abdominal Etching) Performed With VASER?
The core innovation of UAL/VASER is not just fat removal but tissue selectivity. Ultrasonic energy targets fat cells but “does not damage arterial and venous vessels, lymphatics, or fibrous septa (connective tissue).”
This selectivity is what allows the surgeon to perform “high-definition liposculpture” (e.g., a “six-pack” appearance). Traditional SAL is traumatic; working superficially with a SAL cannula can cause significant damage to vessels and connective tissues under the skin, leading to irregularities. VASER preserves these critical non-fat structures, allowing the surgeon to work safely “immediately in the subdermal plane” (just under the skin) and reveal muscular contours.
What Is the “Reconstructive Ladder”?
The “Reconstructive Ladder” is a fundamental concept in plastic surgery for wound closure. It organizes techniques in a hierarchical framework from the simplest to the most complex.
The rungs of this ladder, from simple to complex, are as follows:
- Secondary Intention Healing (Self-closure)
- Primary Closure (Suturing)
- Skin Graft
- Local Flaps (Adjacent tissue)
- Pedicled Flaps
- Free Flaps (Microsurgery)
However, in modern practice, the principle of the “reconstructive elevator” is often used. This means a surgeon may skip simpler steps to choose a more complex option (for example, a free flap for a deep wound on the lower leg) “if it optimizes the outcome.” The goal is not the simplest closure but the most appropriate and durable reconstruction.
What Is the Difference Between a Graft (Skin Graft) and a Flap?
These two terms form the foundation of reconstructive surgery and are often confused.
- Skin Graft: A skin graft is the transfer of skin (epidermis and a variable amount of dermis) that has been completely separated from its blood supply to a recipient wound bed. For the graft to survive (“take”), it must be nourished by diffusion (imbibition) from the underlying wound bed and then grow new blood vessels into the area.
- Flap: A flap is a unit of tissue moved to cover a defect that brings its own blood supply with it (it may include skin, fat, muscle). This blood supply either remains attached to its original site (pedicle) or is connected to a new blood supply via microsurgery.
What Are the Types of Skin Grafts?
There are two main types of skin grafts, and there is a critical clinical difference between them:
- Split-Thickness Skin Graft (STSG – Partial Thickness): Includes the epidermis and part of the dermis. Its advantage is a very high “take” rate and that the donor site (usually the thigh) can heal on its own. It is used to cover large areas (such as burns).
- Full-Thickness Skin Graft (FTSG – Full Thickness): Includes the epidermis and the entire dermis. Its advantage is much better aesthetic and functional outcomes and, most importantly, much less secondary contraction. Its disadvantage is that it is more difficult to “take” (because it is thicker) and the donor site must be closed with sutures, which limits the size of graft that can be harvested.
The clinical choice is a trade-off: STSG provides reliable coverage; FTSG provides high-quality functional/aesthetic reconstruction (especially on the face, hands, and joints).